Top Warning Signs of Cardiac Arrest You Should Never Ignore
Discover the top 10 warning signs of cardiac arrest and why recognizing them early could save your life or someone else’s.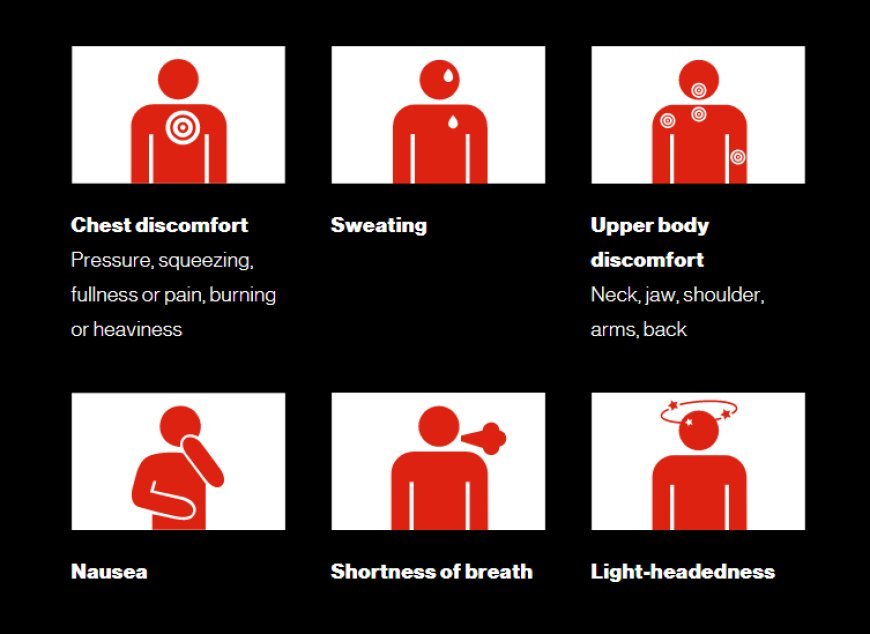
Cardiac arrest is a sudden, life-threatening emergency where the heart unexpectedly stops beating, cutting off blood flow to the brain and other vital organs. Immediate recognition and response are critical because every minute without intervention decreases the chance of survival. While cardiac arrest can occur without warning, there are often signs that appear just before it strikes. Being able to identify these warning signals could mean the difference between life and death. In this article, we’ll explore the top 10 warning signs of cardiac arrest you should never ignore. Understanding these symptoms can help you act fast and potentially save a life.
1. Sudden Loss of Responsiveness
One of the clearest and most urgent warning signs of cardiac arrest is a sudden loss of responsiveness. This happens when the brain stops receiving blood due to the heart’s inability to pump effectively. The person will suddenly collapse, become unresponsive to touch or sound, and may appear lifeless. There is no gradual fade—this is a swift and total shutdown of consciousness.
This is the most defining symptom of cardiac arrest and requires immediate emergency action. Time is critical. Without rapid response, permanent brain damage can occur within minutes. If someone suddenly collapses and is not responsive, you must call emergency services right away and begin cardiopulmonary resuscitation (CPR).
Key signs of sudden unresponsiveness:
- No reaction to shouting or touch
- Limp body with no voluntary movement
- Eyes may remain open or closed but unreactive
- Sudden collapse while engaging in routine activities
2. No Pulse
The absence of a detectable pulse is a major indicator of cardiac arrest. When the heart stops functioning, it fails to pump blood, which results in the complete absence of a pulse. This symptom goes hand in hand with unconsciousness and must be identified quickly, especially by bystanders or first responders.
Checking for a pulse can be challenging if you’re not trained, but in a suspected cardiac arrest, a lack of heartbeat should always be assumed unless proven otherwise. If someone has collapsed, is unresponsive, and isn’t breathing normally, you should assume they are in cardiac arrest and take immediate action.
What to check for when confirming no pulse:
- No pulse felt on the neck (carotid artery)
- No signs of chest movement from breathing
- No audible heartbeat or breathing sounds
- Cold or pale skin
3. Abnormal or No Breathing
Breathing abnormalities are another critical warning sign of cardiac arrest. Right after cardiac arrest begins, the person may experience gasping, also called agonal breathing. This is not normal breathing and should not be confused with signs of life. It’s often irregular, shallow, and may last only a few seconds before breathing completely stops.
Understanding the difference between normal and agonal breathing is essential. Many people hesitate to start CPR because they see the victim gasping and think they’re still breathing. In reality, these gasps are ineffective and indicate a severe medical crisis.
Breathing warning signs include:
- Gasping or gurgling sounds
- Irregular, shallow breaths
- Complete absence of breath
- Blue lips or fingertips (a sign of oxygen deprivation)
4. Chest Pain or Discomfort
Although cardiac arrest happens suddenly, it may be preceded by chest pain or tightness, especially if caused by a heart attack. The pain might feel like pressure, squeezing, or fullness in the center of the chest. This symptom is often a precursor, especially in people with existing heart conditions, and should never be dismissed.
Chest discomfort that lasts more than a few minutes, or goes away and comes back, is a red flag. If chest pain is accompanied by nausea, dizziness, or pain in other parts of the body, immediate medical help is essential. Delaying care increases the risk of cardiac arrest.
Warning characteristics of chest pain:
- Intense pressure or squeezing in the chest
- Pain that radiates to arms, neck, jaw, or back
- Associated with shortness of breath or fatigue
- Occurs at rest or with minimal exertion
5. Rapid or Irregular Heartbeat
A fast or erratic heartbeat can signal that the heart’s electrical system is malfunctioning. Known medically as arrhythmia, this condition can rapidly evolve into cardiac arrest if not treated. Some people describe the sensation as their heart “skipping a beat,” “fluttering,” or “racing.”
While occasional palpitations aren’t always dangerous, a sustained rapid heartbeat or irregular rhythm, especially when accompanied by dizziness or chest pain, should be taken seriously. These symptoms suggest that the heart is not pumping effectively, which may soon lead to collapse.
Symptoms of problematic heart rhythms:
- Palpitations or fluttering in the chest
- Feeling like your heart is “racing” uncontrollably
- Irregular rhythm that comes on suddenly
- Dizziness or fainting along with heartbeat changes
6. Fainting or Near-Fainting
Fainting, or feeling like you’re about to faint, can be a silent warning of cardiac arrest. It suggests a sudden drop in blood flow to the brain, often caused by a significant drop in heart function. In some cases, fainting is the first and only clue that something is wrong with the heart.
Many people dismiss fainting as a result of standing up too fast or dehydration, but when it occurs without a clear cause, particularly in older adults or those with heart disease, it should prompt immediate medical attention.
Red flags for heart-related fainting:
- Occurs during exercise or emotional stress
- Happens suddenly and without warning
- Followed by confusion or weakness
- Recurs frequently or gets worse over time
7. Shortness of Breath
Shortness of breath, especially when experienced without physical exertion, can be a warning sign of impending cardiac arrest. When the heart isn’t functioning properly, oxygenated blood doesn’t circulate efficiently. This leads to a feeling of not getting enough air, even at rest.
This symptom can also indicate congestive heart failure or a precursor to a heart attack—both of which can lead to cardiac arrest. If you or someone else experiences unexplained breathlessness, especially combined with chest pain, dizziness, or fatigue, seek medical help immediately.
Warning symptoms related to breathlessness:
- Sudden onset of breathing difficulty
- Inability to catch your breath, even while resting
- Wheezing or a tight feeling in the chest
- Accompanied by fatigue or chest discomfort
8. Dizziness or Lightheadedness
Feeling dizzy or lightheaded may not seem alarming, but in the context of heart problems, it could be serious. Dizziness often signals that the brain isn’t receiving enough blood, which can happen when the heart is struggling or about to stop.
In many cardiac arrest cases, people report feeling faint or unbalanced moments before losing consciousness. Ignoring this symptom, especially if it occurs repeatedly or alongside palpitations and shortness of breath, can be dangerous.
Symptoms of dizziness to watch for:
- Sudden onset of unsteadiness
- Feeling like you’re going to pass out
- Blurred vision or confusion
- Occurs during activity or rest
9. Unusual Fatigue
Extreme, unexplained fatigue—especially in the days or hours leading up to a cardiac arrest—is a commonly overlooked symptom. This type of fatigue doesn’t improve with rest and is often described as feeling “drained” or “wiped out.”
This warning sign is especially common in women who may not exhibit classic cardiac symptoms like chest pain. When the heart is overworked or failing, it cannot supply enough oxygen-rich blood to muscles and organs, causing severe tiredness.
Signs of concerning fatigue:
- Sudden exhaustion with minimal activity
- Inability to complete daily tasks
- Mental fog or lack of focus
- Accompanied by other symptoms like dizziness or breathlessness
10. Nausea or Vomiting
Though often associated with gastrointestinal issues, nausea and vomiting can sometimes signal cardiac distress. This is especially true if these symptoms appear alongside chest discomfort, dizziness, or cold sweats. The nerves that connect the heart and stomach can cause this “referred” symptom.
In many heart-related emergencies, patients—especially women—may experience nausea and indigestion without recognizing the danger. This symptom is often misdiagnosed, so it’s essential to evaluate it in the context of other warning signs.
Red flags for heart-related nausea:
- Nausea accompanied by chest pain or pressure
- Vomiting with lightheadedness or sweating
- Indigestion not relieved by antacids
- Sudden onset without food poisoning or illness
Conclusion
Recognizing the warning signs of cardiac arrest can save lives. While cardiac arrest often strikes without warning, many cases present symptoms in the minutes, hours, or even days beforehand. Whether it’s sudden loss of responsiveness, chest pain, or unexplained fatigue, knowing what to look for and acting quickly can be the difference between life and death. If you or someone you know experiences any of these symptoms, do not delay. Call emergency services immediately. Education and preparedness are powerful tools in preventing fatalities from cardiac arrest and ensuring the best possible outcomes.
What's Your Reaction?