Cholesterol and Heart Disease: Myths vs. Facts
Busting common misconceptions about cholesterol and heart disease, this article clarifies facts to help you make informed heart-healthy decisions.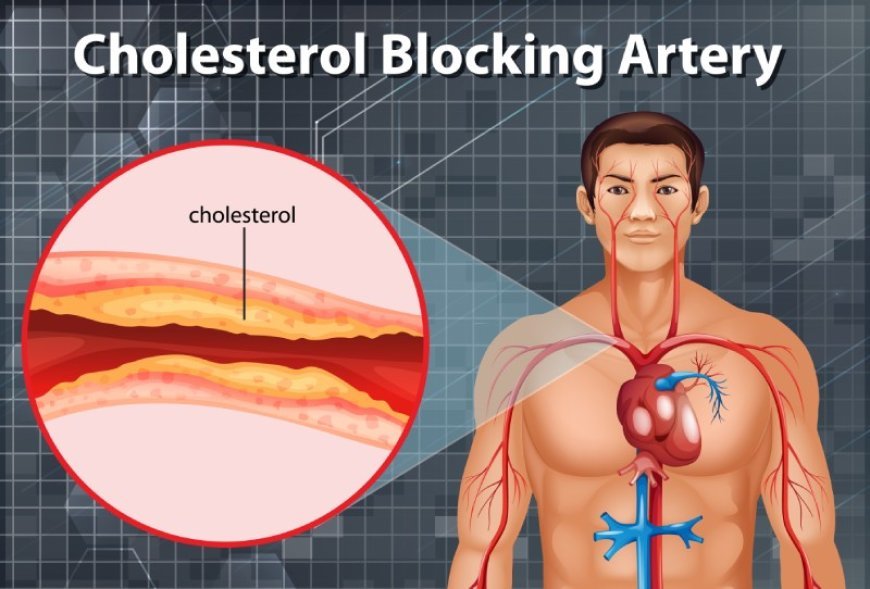
High cholesterol has long been linked to heart disease, but much of what people believe about cholesterol is based on myths and outdated information. This confusion can lead to poor dietary choices, unnecessary anxiety, or neglect of critical risk factors. This article sheds light on ten common myths about cholesterol and heart disease, separating fiction from reality to help you make informed, heart-smart choices. Each myth is countered with clear, science-backed facts to empower you with accurate knowledge.
1. Myth: “All cholesterol is bad for your heart.”
Many people assume that any source of cholesterol automatically puts them at risk for heart disease. The truth is more nuanced. Our bodies need cholesterol: HDL ("good") cholesterol helps clear LDL, while LDL ("bad") cholesterol can lead to arterial plaque buildup. The problem arises when LDL levels become too high, especially when oxidized, and HDL is low. Focusing on overall cholesterol levels without considering their subtypes can obscure important nuances.
Raising HDL through exercise, healthy fats, and quitting smoking improves cholesterol balance. Meanwhile, lowering LDL through diet and medications when necessary addresses the real risk. So not all cholesterol is bad — in fact, HDL cholesterol is protective, and total cholesterol alone is a poor predictor without considering lipid subtypes.
What matters most about cholesterol:
- Balance between HDL (protective) and LDL (potentially harmful)
- Oxidized LDL is especially dangerous
- Triglycerides also play a role in heart risk
2. Myth: "Dietary cholesterol always raises blood cholesterol levels."
For years, eggs and shellfish were branded bad due to high dietary cholesterol. Yet, research shows that for most people, dietary cholesterol has only a modest effect on blood cholesterol. The liver adjusts its production to compensate. In fact, eggs contain nutrients like choline and lutein that contribute to heart and brain health. The 2015–2020 Dietary Guidelines dropped the maximum cholesterol restriction, instead emphasizing saturated fat, sugar, and refined carbs.
Of course, individual responses vary: “hyper-responders” may see more significant blood cholesterol increases from dietary cholesterol. But for most, eating eggs, shrimp, or whole-milk dairy within balanced meals does not elevate heart risk.
Key points about dietary cholesterol:
- Liver adapts cholesterol production
- Saturated and trans fats have greater impact
- Eggs offer beneficial nutrients
3. Myth: “HDL (good cholesterol) can’t be increased.”
It’s often said that HDL levels are fixed and can’t be changed. In reality, lifestyle and even medications can modify HDL. Regular physical activity, especially aerobic exercise, is one of the most effective ways to raise HDL. Additionally, consuming heart-healthy fats—like monounsaturated and polyunsaturated fats found in olive oil, nuts, and fatty fish—contributes to HDL levels. Quitting smoking is another powerful boost.
Certain drugs, like niacin or fibrates, also target HDL. However, raising HDL in isolation hasn’t always reduced heart attack risk. Improving overall cholesterol profiles and reducing inflammation remain the core goal—but yes, HDL can be influenced.
Ways to raise HDL:
- Exercise and maintain healthy weight
- Substitute healthy fats for saturated/trans fats
- Quit smoking and moderate alcohol in women
4. Myth: “Statins are unnecessary and harmful.”
Statins have been controversial, but decades of research confirm their life-saving value. They lower LDL cholesterol and reduce the risk of heart attack, stroke, and death—even in those without symptoms but with risk factors. While they carry side effects like muscle pain or elevated liver enzymes in some users, these are rare, manageable, and far outweighed by the benefits for those at risk.
Statin skeptics often cite bias or disease mongering, but optimal use, dose adjustment, and regular monitoring significantly mitigate risk. For individuals with high LDL, diabetes, or existing cardiovascular disease, skipping statins can be far more dangerous than taking them.
Important facts about statins:
- Cut LDL and inflammation
- Lower heart attack and mortality risk
- Side effects are uncommon and often treatable
5. Myth: “If your cholesterol is normal, your heart is safe.”
Normal cholesterol doesn’t guarantee heart protection. Many heart attacks occur in people with average or slightly elevated cholesterol. Other factors—blood pressure, smoking, diabetes, genetics, and inflammation—play critical roles. Additionally, the size and density of LDL particles matter: small, dense LDL penetrates arteries more easily.
That’s why comprehensive risk assessment—such as the ASCVD calculator—is essential. It evaluates multiple variables, not just cholesterol. Advanced testing like Coronary Calcium Score or C-reactive protein may also identify hidden risk. Cholesterol is one piece of the puzzle, not the whole picture.
Other heart risk factors to consider:
- Blood pressure and smoking status
- Blood sugar, inflammation, and family history
- LDL particle size and arterial calcium scores
6. Myth: “Natural supplements are enough to lower bad cholesterol.”
Supplements like red yeast rice, plant sterols, and omega-3 oils are popular for cholesterol reduction, and some can help modestly. But they’re not a substitute for proven treatments when LDL is high. Red yeast rice contains lovastatin—occasional efficacy, but inconsistent dosing and unregulated quality pose concerns. Plant sterols can lower LDL by 5–10% when taken daily, but evidence doesn’t match statins.
Supplements are best used complementary to lifestyle changes and prescription medication when needed. Relying solely on them when LDL is dangerously high is risky.
Supplement truths to know:
- They help modestly, but are not primary treatments
- Quality and dosing issues exist without regulation
- Should be used alongside diet, exercise, and meds if needed
7. Myth: “Low-fat diets always reduce heart risk.”
Decades of low-fat diet advice focused on reduced total fat, but ignored the type of fat. Many low-fat foods were high in refined carbs and sugar—often worse for lipid profiles. The result? Higher triglycerides and low HDL.
Modern evidence shows that replacing saturated and trans fats with healthy fats improves heart health. Avocados, olive oil, nuts, and fatty fish support cholesterol balance. The key is intelligent fat substitution, not total elimination.
Better dietary fat choices:
- Swap butter for olive oil
- Eat fatty fish twice weekly
- Snack on nuts instead of sugary treats
8. Myth: “Cholesterol only affects older adults.”
No, elevated cholesterol can begin in childhood. High LDL is often hereditary and may run in families. Young people with familial hypercholesterolemia (FH) have extremely high LDL levels from birth and are at serious risk if untreated. Pediatric guidelines now recommend lipid screening from age 9–11, or earlier for those with family history.
Early detection enables interventions: a heart-healthy diet, exercise, and sometimes medications. Starting prevention in youth can dramatically reduce life-long cardiovascular risk.
Why early cholesterol monitoring matters:
- Familial conditions may be genetically driven
- Early lifestyle habits set lifelong trajectories
- Childhood interventions prevent adult heart events
9. Myth: “You can’t eat eggs or shellfish on a cholesterol-lowering diet.”
This outdated idea persists, but evidence doesn’t support it. Dietary cholesterol in eggs modestly affects the blood in most people. Eggs are nutritious: high in protein, choline, lutein, and vitamin D. Likewise, shrimp and shellfish contain healthy nutrients and are low in saturated fat. Replacing processed meats with eggs or shrimp—a healthier protein swap—can improve lipid profiles.
The focus should be on the whole diet, not demonizing foods based solely on cholesterol content.
Smart protein swaps:
- Scrambled eggs vs. bacon
- Shrimp instead of sausage
- Plant-based proteins like beans or tofu also support heart health
10. Myth: “Lifestyle changes don’t matter once you start medication.”
It’s a misconception that taking statins or other drugs frees you to eat what you want. In reality, lifestyle and medication work best together. Healthy habits—for example, a nutrient-rich diet, regular exercise, quitting smoking—enhance drug effects and may lower required doses. Exercise improves HDL and lowers blood pressure; healthy foods stabilize triglycerides and glucose; quitting smoking boosts HDL and reduces clot risk.
Drugs alone don’t address inflammation or metabolic dysfunction. For lasting health, lifestyle must remain central.
Benefits of combining habits and medications:
- Stronger cholesterol and blood pressure control
- Lower medication dosages and side effects
- Faster reduction in inflammation and plaque buildup
Conclusion
Cholesterol and heart disease are more complicated than simple stereotypes. Understanding cholesterol subtypes, dietary effects, treatment options, and individual risk factors is essential for real prevention and health. By debunking these myths and embracing science-based truths—balancing HDL and LDL, eating healthy fats, monitoring young, using medications when needed, and continuing healthy lifestyle habits—you equip yourself to protect your heart. Cholesterol isn’t your enemy; misunderstanding is.
What's Your Reaction?